Why You Should Test for Chronic Infection if You Have an Autoimmune Disease
Infections are caused by an invasion of the body by any external factor that causes damage. These invasions are caused by pathogens, which may take the form of bacteria, viruses, fungi, parasites, or prions.
Acute infections are usually fought off by the immune system, but chronic infections are not removed by the immune system, and can cause health problems for several months, or even years.
Chronic infections are characterized by the presence of flare ups and remissions. The pathogens are present in your body forever regardless if you are experiencing symptoms or not.
For example, if you had the chicken pox as a child, you will have the virus your whole life, but it will go dormant. When you get older, the virus can be reactivated, leading to shingles.
Based on our years of clinical practice and experience, we are guided by the principle that most autoimmune diseases are driven by chronic infections. This is why we don’t merely diagnose a disease, but we look for the underlying infection to get to the real driver of the disease.
Chronic infection examples frequently associated with autoimmune diseases include:
- Anaplasma species
- Babesia species
- Bartonella species
- Borrelia burgdorferi
- Campylobacter jejuni
- Chlamydia pneumonia
- Chlamydia trachomatis
- Coxsackie viruses
- EBV
- ECHO viruses
- Ehrlichia species
- HHV-6
- Hepatitis B
- Hepatitis C
- HPV viruses
- Klebsiella pneumonia
- Mycoplasma pneumonia
- Polyoma viruses
- Streptococcus pyogenes
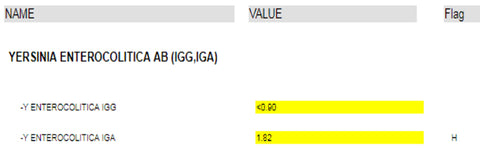
- Yersinia enterocolitica
- Yersinia pseudotuberculosis
Not everyone who gets these infections will develop an autoimmune disease, usually in addition to the infection; some sort of genetic predisposition is involved.
So how do we approach the treatment of autoimmune disease with a chronic infection?
In the therapy of chronic infections there are four goals to achieve.
Goals of therapy
- Symptom control—address the most bothersome problems first and get them under control with drugs, diet, and/or supplements.
- Induction of remission—get the disease to the point of dormancy where you are no longer experiencing negative symptoms.
- Maintenance of remission—remission can remain with drugs, diet, and supplements. Continue to monitor blood work every few months.
- Prevention of flare ups
Can I be cured from chronic infections?
This is one of the most popular questions we get—can I be cured? Complete eradication of microorganisms or viruses causing chronic infections represents an almost impossible task. A more realistic goal of therapy is to induce a dormant state where the infectious process is minimally active and does not induce any clinical symptoms.
This is like the chicken pox example above, it is more likely that you will always have the infection, but a dormant state can be achieved where you are not experiencing symptoms. Tuberculosis is another common example.
How are chronic infections diagnosed?
Where to begin: Labwork
When you are trying to find out what is wrong, you need confirmation from blood work. These results also provide a benchmark to look back on as we progress through treatment.
These are the baseline labs we start with:
Quantitative titers of correspondent antibodies: titers are blood tests that measure whether or not you are immune to a given disease. Quantitative titers give a numerical value indicating your actual degree of immunity to a disease. As opposed to a yes/no value, this gives us the specificity we need to measure disease progression/regression.
Inflammatory markers: these act as a roadmap for disease comparison, we rely on markers for comparison. Examples include elevated CRP (blood test used to detect inflammation) and elevated ESR (a blood test that can reveal inflammatory activity)
Markers of the disease activity
Baseline chemistry: Blood chemistry tests measure certain chemicals in your blood. Results of these tests give your health care provider important information about your general health status, how well organs like the liver and kidneys are working.
NOTE: Use the same lab for testing each time for consistent results.
Additional Factors to Consider During Therapy
Eliminate interfering environmental factors
Heavy metals: If your existing protocol is not responding, there may be heavy metals interfering. Testing for heavy metals is expensive, so it is not for everyone, but can be an effective tool. Examples of heavy metals are arsenic, cadmium, chromium, lead, and mercury.
Immunogenic foods: in susceptible individuals, immunogenic foods produce an undesirable immune response. (Some of these foods include: gluten, dairy, soy, eggs, corn).
Reduce carbohydrate consumption: carbs raise the amount of insulin in your blood leading to prolonged systemic inflammation.
Check and if necessary tune up endocrine functions that should be monitored continuously to prevent the recycling of toxins:
Thyroid function
Adrenal function
Incorporating Antibiotic Therapy
Antibiotics are trying to suppress the proliferation of the offending microorganism. Untreated patients have a very large pool of microorganisms causing harm that their immune system can’t manage. When you take antibiotics this pool shrinks to a small enough size that your immune system can take over and remission happens.
People with chronic infections have microorganisms that go back and forth from dormant to active. Only active microorganisms are killed by antibiotics.
There are several things to consider when choosing antibiotics:
Synthetic antibiotics vs herbal antibiotics: synthetic works faster and more appropriate for issues that need to get under control right away. Herbal antibiotics are a good rout for use on a non-emergent basis and people who prefer this option.
Synergistic antibiotic/herbal combinations: combining traditional antibiotics with dietary supplements can amplify the efficacy of the antibiotic.
Single vs multi-antibiotic therapy: will one antibiotic work, or are multiple needed?
Route of administration: oral, intravenous, or inhaled.
Frequency of antibiotic rotations: you can be on a preset schedule or rotate as one becomes less effective.
Duration of antibiotic therapy: duration can often be from months to years.

