Pseudoappendicitis as Yersinia Enterocolitica
Pseudoappendicitis is any condition that mimics acute appendicitis. A frequent symptom of a Yersinia enterocolitica infection is right lower quadrant abdominal pain, causing Y enterocolitica infections to be misdiagnosed as appendicitis.
Yersiniosis infection is a food-borne illness primarily caused by the bacteria Yersinia enterocolitica. These bacteria are frequently isolated in soil, water, animals, and a variety of foods. Pigs are assumed to be the main carrier of Yersinia enterocolitica.
The most common sources include:
- undercooked pork
- raw chitterlings
- pig intestines
There is an incubation period of 36-48 hours where bacterial replication occurs. Yersinia enterocolitica infection is established via digestion of contaminated food followed by the bacteria crossing the intestinal barrier. The spectrum of disease severity can range from asymptomatic to life-threatening sepsis.
If not treated expeditiously, acute yersiniosis can become a chronic infection.
The predominant symptoms of acute Yersinia enterocolitica infection in humans can include:
- Fever
- Right lower quadrant abdominal pain frequently diagnosed as pseudoappendicitis
- Diarrhea lasting from one to three weeks
- Reactive arthritis can also occur in larger joints appearing 7-14 days after gastrointestinal symptoms and may last for 30-120 days.
- Erythema nodosum with lesions appearing 2-14 days after abdominal pain. Lesions are more common in adult females and usually resolve on their own.
Acute yersiniosis can mimic appendicitis, pseudoappendicitis, and present with right lower quadrant abdominal pain, fever, vomiting, elevated white blood count, and diarrhea.
Patients with pseudoappendicitis taken for appendectomy typically demonstrate inflammation of the terminal ileum and mesenteric lymph node with a normal appendix. Pseudoappendicitis is most common in young children resulting in appendectomy in many cases.
The predominant symptoms of chronic Yersinia enterocolitica infection in humans can include:
- Chronic right lower quadrant abdominal pain
- Recurrent pseudoappendicitis
- Chronic non-traumatic right hip pain
- Chronic right gluteal or sacroiliac pain
- Scoliosis
- Premature osteoporosis
- Reactive arthritis
- Recurrent erythema nodosum
- Avascular necrosis of the hips
Testing for Chronic Yersiniosis
When pseudoappendicitis is suspected, testing for Yersiniosis should be included as part of your lab workup.
Testing can be done on stool, synovial fluid, or serum.
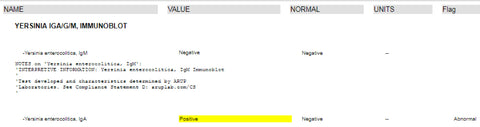
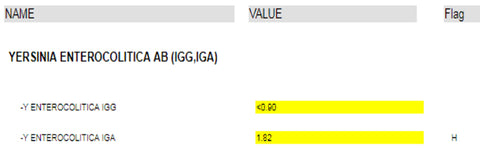
Serum testing is preferred because isolation of the microorganism from the stool or joint/synovial fluid very rarely occurs. Typically, the most reliable test is relied on the demonstration of positive antibodies IgM, IgG and IgA to Yersinia (preferably IgA) in the blood of affected individuals. If IgA is present, this is the greatest indication of an active/aggressive infection—the higher the titer, the more active.
LabCorp and Quest Diagnostics can be used for testing. LabCorp will report a yes/no answer while Quest will provide a numeric value, which provides a more accurate measure of activity.
Quest results:
LabCorp results:
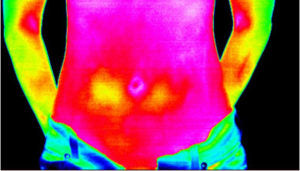
Thermography in Diagnosis of Yersiniosis
Thermography is a non-invasive screening procedure which uses a specialized camera to scan the infrared energy emitted from your body and graphically map and display skin surface temperature visualized in colors.
Thermography is completely safe, has no contact with the body, and uses no radiation. With a yersinia enterocolitica infection, we tend to see a change in surface temperature over the lower right quadrant.
Therapy for Yersiniosis
We have four goals for therapy:
- Reduction of bacterial load
- Correction of inflammatory processes
- Induction of dormant state
- Maintenance of dormancy
As part of therapy, it is our practice to combine both antibiotic and anti-inflammatory drugs. The reason for both is due to inflammation occurring in the lymph nodes, as well as around the mucosal area of the ileocecal valve. Because of this, antibiotics do not penetrate the thickened mucosal area without decreasing the inflammation.
The combination is usually one antibiotic and one anti-inflammatory.
Antibiotic Therapy
Tetracyclines
Azithromycin
Trimethoprim/Sulfomethaxazole
Fluoroquinolones—cannot be used long-term
3rd and 4th generation cephalosporins
Anti-inflammatory Drugs
Sulfasalazine
5-aminosalicylic acid
If left untreated, Yersiniosis will persist indefinitely. For chronic Yersiniosis, you can expect to be in treatment for one year to eradicate the illness.
Dietary Modifications in the Management of Yersiniosis
Low iron diet should be followed because yersinia feeds on iron.
Avoiding Yersinosis
- Avoid raw or under cooked pork
- Store food properly
- Consume only pasteurized dairy products
- Wash hands when preparing food
You are contagious while you have diarrhea and up to three months after diarrhea has stopped. Take extra care to wash your hands to avoid spreading the infection.